Thoracoabdominal aneurysms pose a public health problem that is underestimated in the medical press.
Their prevalence can be deduced from a Swedish study conducted between 1958 and 1985 in a stable urban population with high autopsy rates. They are evaluated at 489 for 100,000 inhabitants. [1] The rate of diagnosis is low. Analysis of the 2009 French PMSI database shows that only 4,000 patients were treated. It is a spontaneously fatal condition and the current surgical or endoluminal treatment results remain sub-optimal.
Conventional treatment of thoracoabdominal aneurysm is surgical, and the principle treatment is flattening of the aneurysm lesion and re-establishment of the continuity using a Dacron prosthesis onto which the visceral arteries are re-implanted.
In addition to the trauma of major surgery and its risks (mortality after treatment remains high: 20% of patients operated on), this operation has to address the difficulty of reliable preoperative identification of medullar vascularisation and therefore identification of the neurological arteries to be re-implanted, and the persistence of aneurysm tissue between the sets of intercostal arteries.
To alleviate these difficulties, two recent alternative techniques have been suggested. The first consists of excluding the aneurysm through a covered stent, with the collaterals being re-implanted separately in the aneurysm area. This procedure may be conducted in two parts and generally reduces post-operative damage. Results recently reported show that this theoretical hypothesis is not confirmed by the facts. [2]
The second technique uses custom-made Dacron fenestrated or branched stents. The morbidity- mortality using this technique is 25% on extended thoracoabdominal aneurysms, with 8% medullar ischaemia, 5% acute renal insufficiency requiring dialysis and 12% intra-hospital mortality. [3].
Post-procedural paraplegia, an improper term as it is associated with major bladder and postural problems, remains an unresolved issue. It occurs in 10% of patients having undergone surgery and 5% of patients treated by endoluminal means. Fenestrated or multi-branched endoprostheses have not changed this rate.
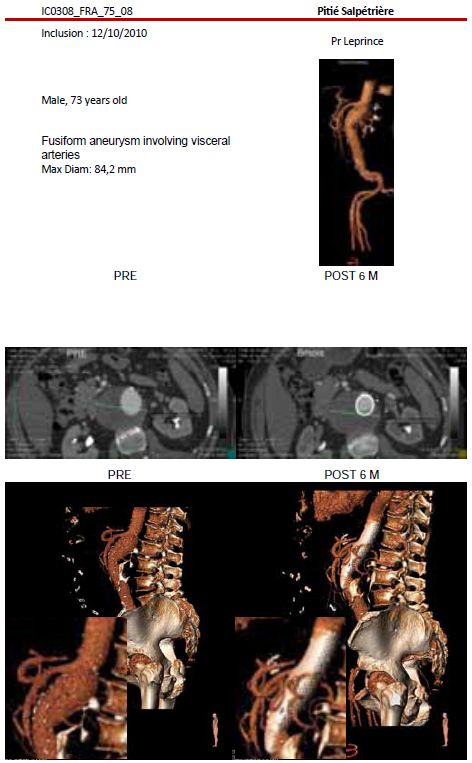
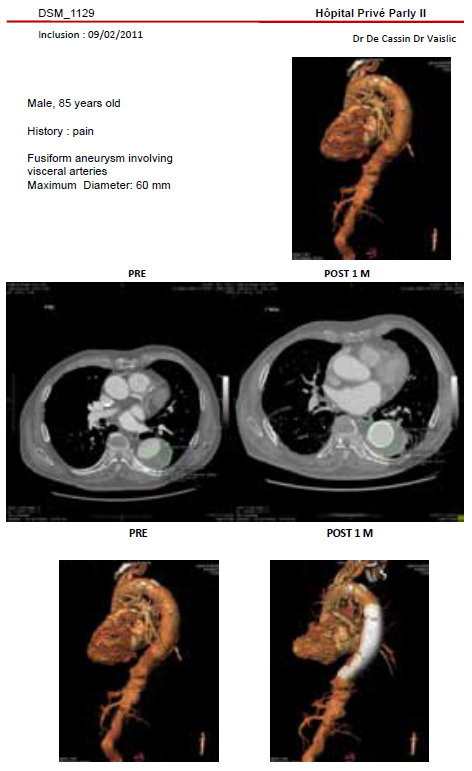
The Multilayer Flow Modulator Technology uses a new concept to laminate the intra-aneurysm flow and reduces critical shear stresses. The Italian prospective multicentre register (52 patients) showed that MFM enables effective treatment of peripheral or visceral aneurysms. 94% of patients recovered within 6 months. [4] The word “recovery” was defined as a stable clinical condition, aneurysm thrombosis, a reduction in the aneurysm diameter and permeability of the collaterals preserved. A Moroccan prospective single centre study was conducted in these 7 patients. This pilot study enabled 85% recoveries after one year.
With the approval of the French health authorities and the ethics committee, a prospective multicentre study was conducted in 9 centres in France among 22 patients with surgical thoracoabdominal aneurysms having been rejected for all other current therapeutic techniques. Monitoring and follow-up was required after one year. At the time of writing, we only have the results presented to the AFSSAPS in October, with feedback of six months.
With this follow up, 60% of the patients aneurysms have been excluded and the remaining have significant reduction and on going healing of their aneurysms. One patient died after three months of documented pneumococcal pneumopathy, four secondary procedures were necessary to correct: a Prostar malfunction, two poorly positioned stents (one of these patients died after 11 months of a cardiac arrest after two CVAs), and an intestinal resection by collateral thrombosis in a patient who was not under double dose platelet antiaggregants; only aspirin had been prescribed.
Out of 170 implants undertaken in 10 countries, no case of paraplegia or medullar ischaemia has been reported.
Conclusion
Based on the limited six month follow up of cases observed in the non randomized French multicentre study results seem satisfactory with 60% of aneurisms excluded and the remaining having reduction in aneurism volume and diameter.
The MFM may represent an alternative to the current treatment of thoracoabdominal aneurysms, enabling exclusion of the sac and preservation of the branches.
The technical problems encountered have made it possible to suggest a number of technical rules: the MFM must not be oversized by more than 25%, the overlap must be greater than 3 cm, the widest device must be placed last and on the inside in order to apply the narrowest one against the wall. Moreover, the primary angioplasty of the branches previously stenosed and the dual platelet antiaggregants are two absolute imperatives. The analysis of the post-operative scan and the correction of any poor positioning are as important as the procedure itself. The mortality and morbidity at six months is 0 if the patient died from pneumopathy is excluded. We have not observed any paraplegia or medullar circulatory insufficiency.
If these results were to be confirmed at one year, this would be a major therapeutic advance in the treatment of thoracoabdominal aneurysms.
References
- 1. Svensjo S., Bengtsson H., Bergqvist D., Thoracic and thoracoabdominal aortic aneurysm and dissection: an investigation based on autopsy, Br J Surg 1996;83:68
- 2. Patel HJ, Upchurch GR Jr, Eliason JL, Criado E, Rectenwald J, Williams DM, Deeb GM. Hybrid debranching with endovascular repair for thoracoabdominal aneurysms: a comparison with open repair. Ann Thorac Surg. 2010 May;89(5):1475-81.
- 3. M. Guillou, B. Maurel Desanlis, J. Sobocinski, P. D’Elia, R. Azzaoui, S. Haulon , Endovascular repair of thoracoabdominal aneurysms Société française de chirurgie thoracique et cardiovasculaire , Lyon Mai 2011
- 4. San Giorgi G.Management of peripheral aneurysms using the cardiatis multilayer stent september 22 nd TCT 2010