About The Heart
How The Heart Works
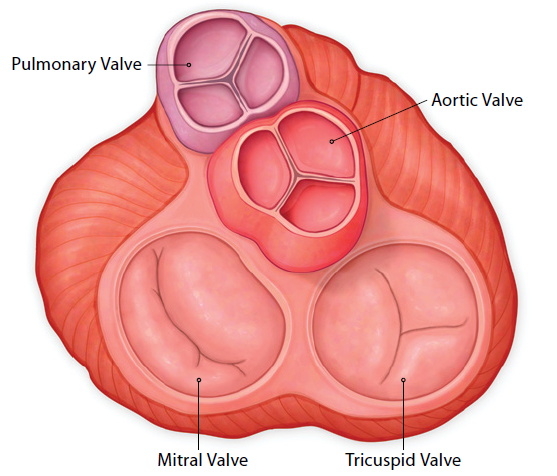
A healthy heart beats approximately 100,000 times a day and pumps about five quarts of blood each minute, or 75 gallons (284 liters) every hour. A normal heart has four chambers. The upper two chambers are the right and left atria. The lower two chambers are the right and left ventricles. The heart’s job is to supply the body with oxygen-rich blood. Blood is pumped through the four chambers with the help of four heart valves — the tricuspid, pulmonary, mitral and aortic valves.
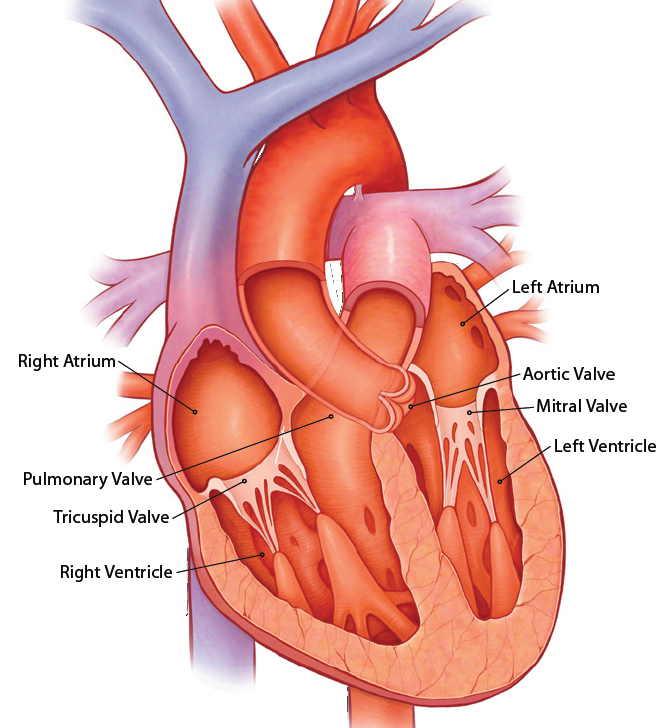
What Heart Valves Do
Heart valves open when the heart pumps to allow blood to flow forward, and close quickly between heartbeats to make sure blood does not flow backward. Any disruption in this normal flow will make it difficult for the heart to effectively pump the blood where it needs to go.The tricuspid valve sits between the right atrium
- (upper chamber) and right ventricle (lower chamber). The tricuspid valve directs blood flow from the right atrium to the right ventricle.
- The pulmonary valve directs blood flow from theright ventricle into the pulmonary artery, which splits into two arteries so that the blood from the body can get to both lungs.
- The mitral valve sits between the left atrium (upper chamber) and left ventricle (lower pumping chamber). The mitral valve directs blood flow from the left atrium into the left ventricle.
- The aortic valve directs blood from the left ventricle into the aorta. The aorta is the major blood vessel that leads from the left ventricle out to the rest of the body.
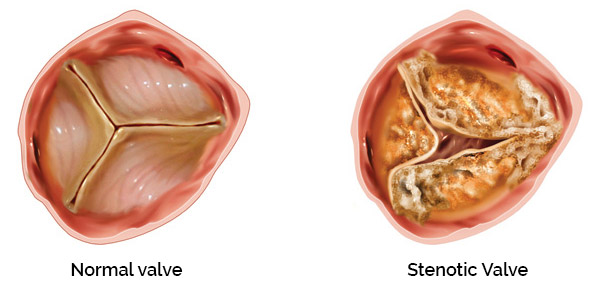
Severe Aortic Stenosis
Severe aortic stenosis (AS) occurs when the aortic valve doesn’t open properly. This forces your heart to work harder to pump blood throughout your body. Over time, the heart muscle weakens. This affects your overall health and keeps you from participating in normal daily activities. Left untreated, severe AS is a very serious, life-threatening condition, leading to heart failure and increased risk for sudden cardiac death.
Causes
Severe AS is often not preventable and may be related to age; buildup of calcium deposits on the aortic valve (stenosis), which causes narrowing; radiation therapy; medications; a history of rheumatic fever or high cholesterol.
Symptoms of Severe AS
Signs and symptoms of severe AS can include:
- Chest pain or tightness
- Feeling faint or fainting with activity
- Dizziness
- Fatigue
- Shortness of breath
- Heart palpitations
- Heart murmur
Treatments for Severe AS—Medical Management
Medical Management and Balloon Valvuloplasty
Medicines for severe AS focus on treating problems that can occur as a result of your diseased aortic heart valve. For example, patients with severe AS may take medicines that help control irregular heartbeats or prevent blood clots. These medicines may help control your symptoms for a period of time; however, without aortic valve replacement, severe AS could worsen to a more serious condition. In addition to medications and if your physician determines appropriate, a procedure called Balloon Valvuloplasty can be performed to relieve symptoms. It is a non-surgical procedure that is performed by placing a balloon into the aortic valve and inflating the balloon. A thin flexible tube (catheter) is first inserted through an artery in the groin or arm and threaded into the heart. Once the tube reaches the narrowed aortic valve, a balloon located on the tip of the catheter is quickly inflated. The balloon presses against the narrowed valve leaflets, which separates and stretches the valve opening and allows more blood to flow through the heart. This procedure does not require open-heart surgery.
Remplacement chirurgical de la valve, intervention à coeur ouvert
Le remplacement chirurgical de la valve aortique par opération à coeur ouvert est un traitement efficace et salvateur pour beaucoup de personnes souffrant d’une sténose aortique sévère. Cependant, environ un tiers de ces personnes ne sont pas éligibles pour un remplacement chirurgical de la valve aortique en raison de leur âge, de leur fragilité ou d’un mauvais état général qui rendent l’intervention chirurgicale trop risquée.
Implantation d’une valve aortique percutanée
L’implantation d’une valve aortique percutanée représente une solution thérapeutique non chirurgicale pour sauver la vie des patients souffrant d’une sténose aortique sévère qui ne sont pas éligibles pour une intervention chirurgicale à coeur ouvert.
Pour l’implantation d’une valve aortique percutanée, un cathéter (petit tube creux) contenant une valve cardiaque spécialement conçue à cet effet est introduit dans une artère de la jambe, puis acheminé jusqu’au coeur. La valve est fabriquée avec un tissu naturel provenant du coeur du porc. Les feuillets qui contrôlent la circulation du sang dans la valve cardiaque sont fixés sur une structure flexible et auto-expansible qui les soutient.
Risks
Because risks will vary depending on your medical management, talk about adverse risk events with your doctor.
Treatments for Severe AS—Open Heart
Open-Heart Surgical Aortic Valve Replacement
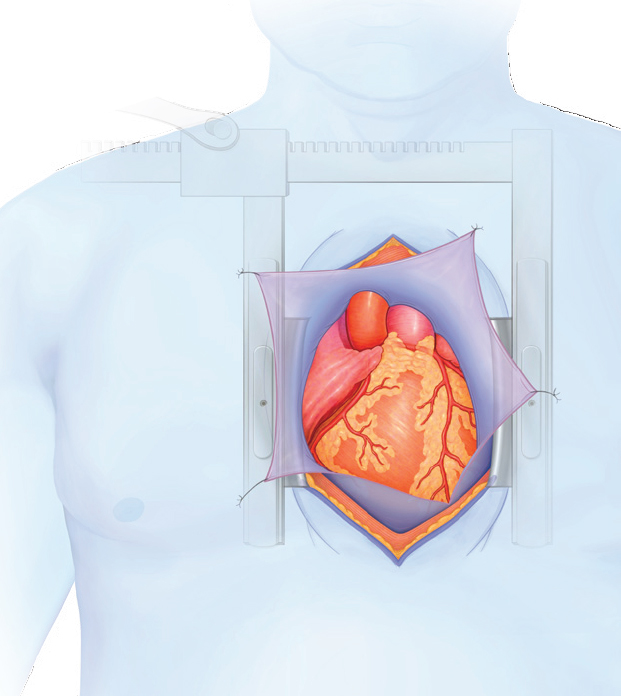
Aortic valve replacement surgery is an effective, life-saving treatment option for people with severe AS. Depending on your risk factors, such as health, diagnosis, and age, your health care providers will be able to recommend the appropriate valve replacement for you. A traditional aortic valve replacement surgery often requires a median sternotomy, where the sternum is split down the middle (some are performed without splitting the sternum). The chest is then opened with special retractors. This provides the surgeon with necessary access to the heart and chest cavity, in order to replace your aortic valve. Because each patient has his or her unique medical history, this information cannot replace discussions with your doctor.
During the Procedure
The operation varies from patient to patient, lasting a minimum of two hours and often longer. During this time, you are asleep under general anesthesia. During the operation, the surgeon will remove any tissue and calcium deposits that are interfering with the normal function of the valve. Your damaged valve may be completely removed. Then, the new valve will be sewn into the space where your own valve used to be. After the surgeon makes sure your valve is working properly, blood flow will be restored to your heart and the incisions will be closed. Your surgery is performed while the function of your heart is taken over by a heart-lung machine (called CPB, for cardiopulmonary bypass).
Implantation d’une valve aortique percutanée
La procédure d’implantation d’une valve aortique percutanée est différente des procédures classiques à coeur ouvert de remplacement de valve aortique.
Le prochain paragraphe décrit le mode opératoire de la procédure d’implantation. Il s’agit d’une présentation générale. Votre situation peut être différente. Vous devez vous rapprocher de votre médecin pour discuter des détails spécifiques de l’intervention.
After the Surgery
Immediately after the operation, you’ll probably be drowsy. You will spend the next few hours, or possibly the night, in the intensive care unit. When intensive care monitoring is no longer needed, you will be moved to a step-down unit and eventually to a routine-care hospital floor. A typical hospital stay is 5-10 days. After you’re released from the hospital, you will need to see your doctor periodically for follow-up visits.
Summary of Open-Heart Surgical Aortic Valve Replacement
- General anesthesia
- Patient on heart-lung bypass machine
- Chest open, 7-inch incision (often, but alternatives exist)
- Valve replaced during 2-4 hour procedure (typical)
- 5-10 day hospital stay (typical)
- Approximately 6-8 week recovery period
Procedural Overview of a Typical Open-Heart Surgery
- 1. Patient is administered general anesthesia to remain asleep and pain free during the procedure.
- 2. After preparation, an incision to access the heart is made.
- 3. The patient is connected to a heart-lung machine to isolate the heart.
- 4. The old valve is removed.
- 5. A new valve is placed.
- 6. The patient is weaned from cardiopulmonary bypass.
- 7. Your new aortic heart valve will begin working. The doctor will conduct a test to confirm the valve is working properly.
- 8. All incisions are closed.
- 9. Patient is transferred to ICU and kept on ventilator until deemed ready to remove.
Potential Risks for Surgical Aortic Valve Replacement
Valve replacement can include the following risks:
- Death.
- Blood clots that develop in the heart or on the replacement valve. These clots may break loose and travel through the bloodstream (thromboembolism). This problem may cause a stroke or heart attack.
- Obstruction of blood circulation to the heart resulting in damage to the heart tissue (myocardial infarction).
- Angina.
- Abnormal heart beat (cardiac arrhythmia and dysrhythmia).
- Heart failure.
- Damage to red blood cells (hemolysis) that can result in anemia.
- Blood leaking around the outside of the prosthetic valve (paravalvular leak) or any problem with the valve that causes leaking of blood after the valve has closed (transvalvular leak).
- Any problem with the prosthetic valve that causes narrowing of the valve opening (stenosis).
- Failure of the valve to open and close properly. Inflammation of the lining of the heart (endocarditis).
The potential risks are shown in the order of severity, from most severe to least severe. This list is not inclusive of all risks. Talk to your physician regarding more information about aortic valve replacement surgery.
Treatments for Severe AS—CoreValve
CoreValve® Transcatheter Aortic Valve Implantation (TAVI)
The CoreValve aortic heart valve is made of natural tissue obtained from the heart of a pig. The leaflets that control the flow of blood in the CoreValve heart valve are secured to a flexible, self-expanding frame for support. With CoreValve TAVI, an incision is made and a new aortic valve is delivered via a catheter. It is a less invasive treatment option than open-heart valve surgery.
During the Procedure
Patients may be sedated during the 1-3 hour procedure. You may first have a test that uses sound waves to take a closer look at the inside structures of the heart. With CoreValve TAVI, a catheter (thin, hollow tube) holding a specially designed heart valve is guided to the heart. Special imaging equipment is used to guide position and placement of the CoreValve aortic heart valve.
After the Procedure
Following CoreValve TAVI, you will be moved to an intensive care unit or cardiac care unit. Patients typically are able to be up and walking within 24-48 hours after their procedure. Your doctor will determine when you are ready to move to a standard hospital room. The typical hospital stay for CoreValve TAVI is 3-5 days.
Summary of CoreValve TAVI
- Local or general anesthesia
- Heart pumps normally
- Catheter delivers valve to heart
- Valve replaced during 1-3 hour procedure (typical)
- 3-5 day hospital stay (typical)
- Approximately 1-week recovery period
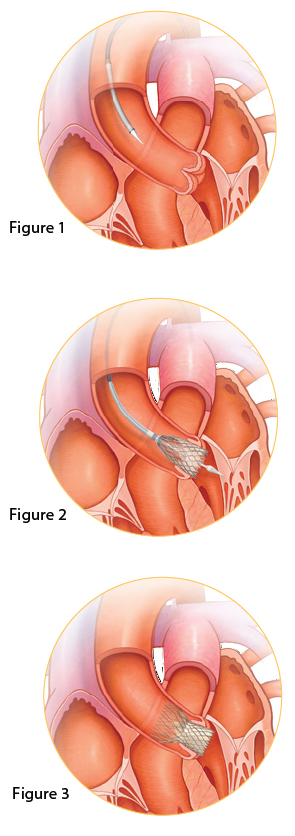
Procedural Overview of a Typical CoreValve®
- 1. Patients are normally sedated during the approximately 1-3 hour procedure. Because each patient is different, your doctor may determine whether or not you should be fully asleep for the procedure.
- 2. The interventional cardiologist or cardiac surgeon will make an incision and guide a sheath (long, hollow tube into your heart. (Figure 1)
- 3. Using special imaging equipment to look at your arteries, a catheter with a balloon on the tip is threaded through the sheath and into your heart. If you’re not fully sedated, you may have a “fluttering” feeling in your chest. This is caused by extra heartbeats occurring once the catheter is in your heart.
- 4. When the end of the balloon is in your aortic valve, the balloon will be inflated and will force your narrowed aortic valve open to prepare it for your CoreValve aortic heart valve.
- 5. Again, using the special imaging equipment, your doctor will place the CoreValve aortic heart valve in position over your own diseased aortic valve. (Figure 2)
- 6. Your new aortic heart valve will begin working. The doctor will conduct a test to confirm the valve is working properly. (Figure 3)
- 7. The catheter will be removed, the incision will be closed, and the procedure will be complete.
Potential Risks for CoreValve® Implantation
Implantation of the CoreValve Transcatheter Valve may include the following risks:
- Death including all cause and cardiovascular mortality
- Myocardial infarction including coronary occlusion
- Stroke including permanent stroke and TIA
- Re-intervention including sAVR and repeat valve placement
- Aortic regurgitation
- Permanent pacemaker placement
- Pericardial tamponade (wire perforations)
- Vascular and bleeding complications
- Valve migration or fracture
The potential risks are shown in the order of severity from most severe to least severe. This list is not inclusive of all risks. For a complete listing of possible risks and discomforts, talk with your doctor.
Follow-up Care
Your doctor will provide you with more specific care instructions as well as any restrictions you may have. You will still need to take any medications as prescribed and have your heart and valve function checked from time to time. Ask your heart doctor or nurse about your follow-up appointment schedule or any other questions you have about living with your new heart valve. As a precaution, you’ll want to inform your dentist and other doctors about your heart valve before any dentist or medical procedure. If you require a magnetic resonance imaging (MRI) scan, tell the doctor or MRI technician that you have had a heart valve procedure. It is important to keep appointments with your heart doctor and to follow recommended daily care to ensure the best possible results.
Is CoreValve® Right For You?
CoreValve Transcatheter Aortic Valve Implantation may be right for you if you have been diagnosed with severe aortic stenosis but your doctor has determined that you are not a candidate for openheart valve replacement surgery. CoreValve is not right for everyone. Your doctor can help decide if CoreValve may be right for you. For more information on this new, non-surgical treatment for severe aortic atenosis, visit www.CoreValve.com.
CoreValve Transcatheter Aortic Valve Benefits
Symptom Relief
Most patients receiving a CoreValve heart valve can expect immediate symptom relief. In several studies, more than 80% of patients reported symptomatic improvements of at least one NYHA heart failure class after their procedure.*
Quality of Life Improvements
Patients also reported significant improvements in quality of life measurements,† including:
- Vitality
- Emotional well-being
- Social activities
- Physical activities
- Bodily pain
*Data on file, Medtronic, Inc.
Frequently Asked Questions
- Are physical activities safe?
Discuss your activity level with your heart doctor to determine what is best for you. - Is it safe to have an x-ray with a CoreValve® aortic heart valve?
The CoreValve aortic heart valve is completely safe with x-ray examinations. - Is it safe to have an MRI with a CoreValve aortic heart valve?
The CoreValve can be safely scanned under certain conditions. Inform your physician about your implanted transcatheter valve prior to having an MRI. - How will I know if my CoreValve aortic heart valve is working properly?
Your heart doctor will schedule regular follow-up appointments to check your valve. - How long will my CoreValve aortic heart valve last?
The CoreValve device has been tested in laboratory for the same duration as our surgical prosthetic heart valves. Because of the uniqueness of each heart patient, it is difficult to predict how long the CoreValve aortic heart valve will last.
Online Resources
For more information on aortic stenosis visit the following web sites:
- CoreValve Transcatheter Aortic Valve Implantation, www.CoreValve.com
- WebMD, http://www.webmd.com
- MayoClinic.com, http://www.mayoclinic.com
- American Heart Association, www.americanheart.org