I – Defining atherosclerosis
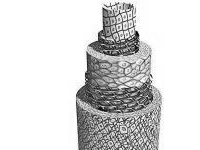
Atherosclerosis is the loss of artery compliance due to sclerosis, the latter caused by a build-up of fatty materials (mainly the « bad » cholesterol, LDL) on the inner layer of the arteries, the tunica intima. This build-up forms an atheroma, which can vary from a fatty streak narrowing the arterial lumen to a lesion completely blocking the vessel. These two conditions are known as stenosis and thrombosis, respectively.First, it is useful to understand the structure of arteries. Arteries are made up of three layers, or “tunicae”. The tunica intima is the innermost layer in direct contact with the blood. The tunica media is the middle layer, made up of smooth muscle cells that promote vessel compliance. Finally, the tunica externa, or adventitia, is mainly made up of connective tissue.Although an atheroma can form in any of the body’s arteries, medium and large arteries are the most prone: the aorta, the arteries of the limbs, the carotids, and the renal, coronary, and digestive arteries.
The atheroma gradually calcifies the intima and media, building up calcium carbonate deposits and LDL cholesterol crystals.
This thickening of the wall and narrowing of the lumen may gradually obstruct the artery, cutting off oxygen to the organ supplied by this artery.The pathology develops as follows. The initially smooth fatty streak can become ulcerated, causing either small clots to accumulate or debris to migrate upstream from the atheromatous plaque. At a later stage, smooth muscle cells migrate from the tunica media to the tunica intima, progressively obstructing the arterial lumen. This impaired blood circulation causes ischemia in various areas of the body (brain, heart, limbs, or visceral organs), and the lack of blood causes infarction (tissue death).
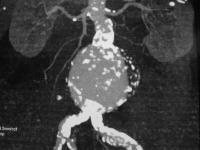
Sometimes, through the rupture and necrosis of the tunica media, the atheroma causes the artery to gradually dilate, leading to an aneurysm. Aneurysms are most commonly found in the abdominal aorta, below the renal arteries.
Atherosclerosis is quite common. Its pathology was described in 1904 by Félix Marchand of Leipzig. Called arteriosclerosis when it affects medium and large arteries, it should not be confused with another condition that similarly modifies the arteries, arteriolosclerosis. This second condition affects the small arteries and arterioles, and aging is the main risk factor. The combination of both explains the growing number of elderly subjects suffering from arteritis, threatening the viability of a limb.
II- Causes and most affected populations
- A sedentary lifestyle and obesity are two of the top cardiovascular risk factors, along with smoking.
- Comorbidity factors contributing to the development of atherosclerosis are arterial hypertension (high blood pressure), dyslipidaemia with a high LDL cholesterol count, and type 2 diabetes (sometimes called adult onset diabetes).
- Heredity and stress are also involved in the appearance of this condition which affects more men than women, and whose frequency increase with age.Atherosclerosis affects the majority of elderly “Western” populations, being responsible for 40% of mortality – the leading cause of death for this demographic.
Conditions caused by atherosclerosis are essentially distinguished by the organ affected:
- heart
- brain
- aorta and its main visceral branches leading to the kidneys, liver, and intestine
- lower limbs
III – Symptoms
Symptoms differ depending on the arterial territory affected, with the pathology proportional to the degree of narrowing caused by the atheroma.
- In the heart, stenosis (i.e. narrowing) of a coronary artery can cause chest pain called angina or angor pectoris, at rest or during exertion, while obstruction or occlusion of the artery (called thrombosis) will cause acute coronary syndrome or myocardial infarction.
- In the brain, uneven plaque or tight stenosis in a carotid artery can cause a transitory ischemic attack or “mini-stroke”, so-called since it only lasts for a few minutes to an hour. This can cause loss of vision in one eye or motor or sensory dysfunction in an upper limb, lower limb, or on one side of the body. At a more advanced stage, it can cause a stroke, causing infarction in a region of the brain, with or without major clinical damage.
- In the arms and legs, stenosis or arterial occlusion causes ischemia in the arterial territory during physical exertion. This is called intermittent claudication. The pain is relieved by rest. The development of a back-up circulation called “collateral circulation” plays an important role, and can delay the appearance of symptoms. The absence of collateral circulation, or the distal topography of the atheroma, can cause pain even at rest, making the ischemia more serious. In some cases, the ischemia can be acute and require emergency care.
In the latter stages, known as critical limb ischemia (CLI), the development of localized necrosis of the toes and foot signals a distal occlusion of the neighbouring arteries. This can lead to gangrene, endangering the viability of the limb and carrying the risk of amputation. This is the last stage of arteritis.
IV – Risks
Atheromas are the leading cause of most cardiovascular conditions, endangering not only a sufferer’s life (atherosclerosis is responsible for 40% of mortality in developed countries) but also quality of life, given the functional repercussions on affected organs:
- Heart failure from ischemia arising from damage to the coronary arteries. This considerably alters quality of life, ruling out almost all physical exertion.
- Insufficient blood circulation to the brain from a single or multiple strokes, with resulting hemiplegic damage, speech problems, or dementia.
- Peripheral vascular disease or arteritis (arterial inflammation). Left untreated, this can lead to the amputation of one or both limbs, above or below the knee, with terrible consequences in terms of functional incapacity.
- Kidney failure due to damaged renal arteries. This can lead to the need for haemodialysis (circulating blood through an artificial kidney).
- Inadequate intestinal circulation from damage to the digestive arteries, with a very serious risk of mesenteric infarction.
V – Main exams
Any functional discomfort requires a careful clinical examination and precise history taking: arteritis of the lower limbs starts with the appearance of muscle cramps during exercise, then muscle pain that interferes with walking, known as intermittent claudication. In the next stage, pains appear while lying down, forcing sufferers to leave one leg outside their bed. Next, the pain becomes chronic and interferes with sleep. In the last stage, lesions called “trophic changes” appear on the toes or foot, progressing from superficial necrosis to gangrene. In a clinical examination, the general practitioner will palpate for a peripheral pulse, listen for an abnormal whistle indicating stenosis on an arterial vessel, and take the patient’s blood pressure to look for abnormally high blood pressure.
- An annual blood and urine test is indicated in cases of obesity (to detect diabetes) and family history of cardiovascular problems. This test determines uric acid levels and levels of lipids such as LDL cholesterol and triglycerides.
- A Doppler ultrasound of the aorta, peripheral arteries, and the arteries supplying the brain (carotids) as soon as the patient presents either classic symptoms of arteritis of the lower limbs or a mini-stroke. More systematically, a Doppler ultrasound is recommended for patients over 40 years old presenting at least three cardiovascular risk factors, such as hypertension, smoking, dyslipidaemia, obesity, diabetes, a sedentary lifestyle, stress, and family history.
- The opinion of a specialized cardiologist is absolutely necessary, along with appropriate exams, in all patients with atherosclerosis, particularly before surgery.
- A specialist consultation with a vascular surgeon if an atheroma has been discovered. Depending on the type of lesion, its topography and its clinical effects, the specialist will ask for exams to help choose a course of treatment, as well as additional imaging ranging from an angiogram to an angio MRI (with the current trend being towards the least invasive exams).
VI – Main treatments and their risks
Prevention is still the main treatment:
- quit smoking
- exercise more
- control blood pressure
- correct dyslipidaemia
- control diabetes
- lose weight through proper nutrition
Medical treatment mainly includes:
- Antiplatelets, such as small doses of aspirin or clopidogrel, to reduce clotting from an atheroma.
- Statins to normalize LDL cholesterol and lipid levels (along with a low-fat diet).
- Blood pressure medication (if applicable), mainly angiotensin-converting-enzyme inhibitors (ACE) and calcium blockers.
Open or endovascular repair are performed if the condition is life-threatening, causes major functional disturbance, or significantly jeopardizes the viability of an organ or limb.
Several surgical techniques aim to restore the arterial lumen, restore blood supply to the deprived area, or eliminate the arterial aneurysm:
- Balloon angioplasty uses a balloon catheter to dilate the lumen, with or without a stent, to correct stenosis and recannulate a short arterial blockage.
- Endarterectomy is the surgical removal of the atheromatous plaque blocking the artery, opening up the lumen and leaving only the tunica externa.
- Arterial bypass, which as its name suggests, “bridges” the blocked artery allowing blood to flow from the healthy artery upstream to the patent artery downstream. The bypass graft may be made from a vein, artery, or synthetic material.
Two techniques are used for aneurysms: a graft bypass through conventional open surgery, removing the aneurysm, or a covered stent graft that excludes the aneurysm.
In all cases, the risks must be weighed against the benefits of each technique and thoroughly explained to the patient beforehand. Each operation must be adapted to the individual, taking into account their NYHA functional class, overall health, and biological age (more so than their real age).
VII – Medical follow-up
Follow-up must be regular, including clinical exams and biomonitoring based on the types of medicine being taken, such as the blood thinners that are sometimes required after a bypass. The exams also include a regular Doppler ultrasound after one month, six months, then yearly following angioplasty or open surgery, in order to track changes to the atheroma or detect any deteriorations to the operated areas.
Only the vascular surgeon is able to recommend more specific exams such as angiograms or angio MRIs during the yearly check-up.
Conclusion
Atherosclerosis is a very common disease and the leading cause of death in developed nations. Prevention mainly includes eating a balanced diet, getting regular physical exercise, avoiding tobacco and alcohol use, monitoring blood pressure, and treating diabetes or high cholesterol.
Glossary
aneurysm:
localized dilation of the artery wall leading to the formation of a pocket, usually spherical in shape, which can reach a diameter of several centimetres.
angina:
see angor pectoris
angioplasty:
surgical technique most often performed by puncturing the skin above an artery and introducing a guidewire with a balloon to dilate the narrowed passage of an artery (stenosis) or recannulate a blocked artery segment (thrombosis) (also called percutaneous coronary intervention or PCI).
angor pectoris:
chest pain (also called angina) often felt also in the left arm and jaw, which arises at rest or during exertion and which indicates an atheroma affecting the heart arteries (coronary arteries).
antiplatelets:
medication that reduces clot formation and platelet adhesion. Platelets are blood cells that play a role in primary haemostasis. Antiplatelets are not blood thinners. The most commonly used antiplatelets are aspirin and clopidogrel.
aorta:
the largest artery of the human body. It arises from the heart’s left ventricle and carries oxygenated blood to the rest of the body, the brain, the visceral organs, and the limbs.
arterial hypertension:
high blood pressure. Blood pressure is considered normal when the first figure (systolic pressure when the heart is contracting) is under 140 mm of mercury and/or when the second figure (diastolic pressure when the heart is relaxing) is under 90 mm of mercury.
arteritis:
inflammation that gradually obstructs the arteries of the lower limbs (also called peripheral vascular disease; linked to atherosclerosis).

atheroma:
sedimentary build-up of fatty and calcific deposits on the tunica intima of medium and large arteries, leading to a thickening of the artery wall that can lead to a blockage of the artery.
Atheromas are an affliction of the arteries linked to the formation of fatty plaque that gradually blocks the arteries. If they break away or fissure, these build-ups can cause the appearance of a blood clot which will block the vessel.
cardiovascular risk factors:
elements that contribute to atherosclerosis and cardiovascular illnesses. Principal risk factors include high blood pressure, elevated cholesterol levels, smoking, diabetes, a sedentary lifestyle, obesity, stress, heredity, and age.
carotid arteries:
the two main arteries of the neck, supplying blood to the brain along with the vertebral arteries.
cholesterol:
one of the fats (lipids) carried by the blood. Too much « bad » cholesterol (i.e. LDL, or low density lipoproteins) is one of the factors contributing to the formation of atheromatous plaque.
claudication:
a cramp-like pain in the calf, thigh, or buttock felt while walking, and which signals the narrowing or occlusion of an artery cutting off blood upstream from the painful area. It is called intermittent claudication if the pain stops when the sufferer stops walking.
coronary arteries:
the arteries that supply blood to the heart muscle or “myocardium”. They are the first branches of the aorta, and derive their name from the Latin for « crown », describing the way they surround the heart.
diabetes:
chronic illness affecting the regulation of blood sugar (blood glucose) levels due to insufficient insulin production in the pancreas.
Doppler ultrasound:
painless exam using ultrasound waves to assess blood flow in the vessels and diagnose narrowing (stenosis) or occlusion (thrombosis), mainly in the arteries of the neck, the aorta, and the peripheral arteries in the limbs.
dyslipidaemia:
disorder in which the body cannot metabolise lipids (fats) and which leads to overly elevated “bad” cholesterol levels (LDL) and/or triglycerides. – high blood pressure: see arterial hypertension
infarction:
sudden, massive cell death causing irreversible necrosis to part of an organ and arising from a lack of oxygen and the occlusion of the artery supplying blood to the area. Some examples are myocardial infarction, cerebral infarction (ischemic stroke), renal infarction, and bowel infarction (from occlusion of the mesenteric arteries).
ischemia:
a shortage of oxygen supplied to an organ or other part of the body. The lack of oxygen disrupts and may even stop the organ’s functioning. Ischemia is a vascular emergency that may be reversible if treated in time. However, it is irreversible if left too long and leads to infarction in organs or gangrene in limbs.
lipids:
the fatty materials of living beings. Cholesterol is a lipid.
peripheral arteries:
vessels carrying blood oxygenated by the lungs towards the outer regions of the body, particularly the arms and legs.
peripheral vascular disease:
see arteritis
symptom:
a subjective or objective manifestation of an illness as expressed by a patient or observed by a physician.
thrombosis:
obstruction of a blood vessel (artery or vein) by a blood clot. To a greater or lesser extent, this is the final stage of atherosclerosis in an artery.
tunica adventitia:
see tunica externa
tunica externa:
outer layer of the blood vessels made up of relatively resistant fibrous and elastic connective tissue (also called tunica adventitia).
tunica intima:
internal layer of the blood vessel that comes into direct contact with circulating blood.
tunica media:
the middle, muscular layer of the artery wall, located between the tunica intima and the tunica externa. It ensures the vessel’s vasomotor action (contracting and dilating).